TMJ and TMD – Jaw Pain
Who should get TMJ, TMD or MSD Therapy?
If you are experiencing pain around your jaw joint area please review the TMJ-TMD-SIGNS AND SYMPTOMS form. If you have some of the signs and symptoms, print the form, and bring the TMJ-TMD-QUESTIONNAIRE completed to your first appointment. We would like to recommend for you to read “What’s the fee” for the initial TMJ/TMD exam? If you are experiencing more then one of the symptoms on our form, contact us to schedule an appointment. When you come to our office Dr. David Alpan will review these two forms, do an oral and physical exam, ask you more questions and then discuss some options for you.
What are signs?
These are what the trained health practitioner finds during the examination. Usually the patient being examined is unaware of signs.
What are symptoms?
This is what the patient is aware of and tells the therapist. Many people live with symptoms without complaint thinking they are normal because they do not hurt or bother them enough.
If you have chronic pain, putting off the initial TMJ examination, may result in more symptoms and more severe pain. As the body adapts, many of these signs and symptoms get harder and more costly to relieve or eliminate.
At the top of the page, click on Request an Appointment Online; then print and complete the TMJ-TMD-QUESTIONNAIRE and the NEW PATIENT INFO AND HEALTH QUESTIONNAIRE and bring these forms with you to your first appointment.
What is TMD?
TMD stands for Temporal Mandibular Disorder, which describes an incorrect relationship of the mandible (lower jaw) to the temporal bones on the left and right side of the skull. It is commonly referred to as a “TMJ problem.” The muscles in the face move the lower jaw when you speak, yawn, chew and swallow. The lower jaw has a special relationship with the upper jaw and temporal bones. When this relationship is abnormal, chronic pain in the face, head, neck, shoulders, jaw joint, etc, may occur. Your teeth and bite support the facial muscles in this special relationship.
What causes TMD? One or more of the following may cause TMD:
- Mal-occlusion (bad bite) forces muscles in the face to strain while speaking, chewing and swallowing -many people can adapt to this bad bite without any apparent signs or symptoms.
- Pressure on the skull bones during birthing and by the doctor assisting the birthing process.
- Genetics passed from grandparents and parents to their children.
- Sleeping patterns during growth and development years.
- Trauma from falling, car accidents (whiplash), being struck by a person or object.
- Arthritis or other illnesses. Emotional trauma can also cause symptoms or aggravate existing TMD symptoms. There are over 150 symptoms associated with TMJ/TMD problems.
TMD can be accompanied by pain or discomfort and can inhibit your ability to perform daily tasks normally. While we strongly recommend seeking professional care for TMJ and TMD, Dr. Alpan does recommend the following tips for alleviating TMD-related discomfort.
What is TMJ?
TMJ stands for Temporal Mandibular Joint or jaw joint. This is the joint where the mandible (lower jaw) articulates (hinges) with the temporal bones on both sides of the skull. A disc in this joint separates the mandible from the temporal bones. When you speak, yawn, chew or swallow, this is where the lower jaw articulates with the temporal bones. The jaw joints can be found with your fingers when you open and close your mouth. They are just in front of your ears.
“TMJ” is used to communicate with the general public regarding the many signs and symptoms in the jaw joint (TMJ), and the head, neck and muscles in the face (TMD). Some TMJ Therapists lump the signs and symptoms in the jaw joint, head, neck and the facial muscles together and call it TMD. TMJ and TMD signs and symptoms are included in the TMJ-TMD SIGNS AND SYMPTOMS form and the TMJ-TMD-MSD QUESTIONNAIRE form.
What is TMJ Therapy at Alpan Orthodontics?
The technology used by Dr. David Alpan to diagnose and treat TMJ/TMD signs and symptoms was developed in the 1960’s by Bernard Jankelson, DDS, in Seattle, Washington. Dr. Jankelson developed the Myomonitor, an electronic device, to assist TMJ Therapy. He then founded Myotronics, the organization that continues to educate dental and medical professionals about diagnosing and treating these disorders. Robert Jankelson, DDS, continues the work of his father in Myotronics where they continue researching and developing newer and better technologies for TMJ/TMD diagnosis and treatment.

Dr. David Alpan’s father, Jack Alpan, DDS, NMD (a general dentist from 1960-1997) learned directly from Dr. Bernard Jankelson in 1973 at the University of Southern California School of Dentistry in Los Angeles, where Dr. Jack got his DDS degree. Dr. Jack began diagnosing and treating his patients with TMJ/TMD problems. He helped approximately 2,000 patients during those twenty-four years, relieve or totally eliminate many of their symptoms. Dr. Jack told Dr. David about these patients’ success stories during his formative years. Dr. Jack conveyed how much personal satisfaction he got from relieving or eliminating so many of the symptoms and improving their lives.
Dr. David began to formulate his own TMJ treatment, based on his father’s success with Dr. Jankelson’s technology. Dr. David was also mentored and influenced by Dr. Chase at the University of the Pacific (UOP) School of Dentistry in San Francisco. Dr. David attended many postgraduate classes at Myotronics and earned the Master of Science in Dentistry (MSD) degree for writing his Master’s Thesis on TMD research during his two year orthodontic specialty training at UOP School of Dentistry. He has been practicing TMJ therapy in private practice since 1999, when he founded Alpan Orthodontics in Los Angeles & Beverly Hills.
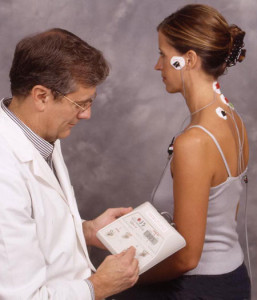
The following explains the function of the Myomonitor, a TENS device, used in TMJ Therapy:

Myomonitor (muscle monitor) is the electronic device used to relax the muscles in your face in order to relieve muscle strain that results in signs and symptoms. It is powered by a nine-volt battery. The scientific name for this device is a Transcutaneous Electronic Neuromuscular Stimulator (TENS). The TENS device is attached to leads, which are attached to both sides of your face and neck. When it is turned on, it sends a painless electronic impulse through the leads to stimulate the nerves in the face, which contract the muscles in the face that move the lower jaw. There are 42 contractions and relaxation cycles per minute. This causes the brain to release endorphins – natural hormones that relax the muscles. After pulsing for 90 minutes, the muscles become more relaxed. Many people notice that the lower jaw has moved to a new position, or maybe not. If the lower jaw does move into a new position, the teeth now come together differently while on the Myomonitor than before the TENS treatment began. This neuro-muscular bite is different from the accommodated bite, which the patient adapted to and which may be causing the signs and symptoms of TMJ/TMD.
If Dr. David Alpan recommends 1-3 TENS treatments, and there is no change in the relationship of the lower to upper jaw and there is no alleviation or elimination of your symptoms, he will discuss other options, or refer you to another health-care provider.
What is the initial TMJ exam, TMD exam or MSD exam?
- A review of your signs and symptoms
- A review of your MSD-TMD-TMJ QUESTIONNAIRE and your New Patient Info & Health Questionnaire
- An oral and physical exam
- A diagnosis and treatment plan
- Cancer Screening Exam
If you need TMJ/TMD therapy, Dr. David Alpan will evaluate exactly how long you will be in treatment. 1-3 TENS treatments may alleviate or eliminate your symptoms. Occasionally 1-3 TENS treatments with minor tooth adjustments alleviates or eliminates symptoms. If these procedures don’t help you, Dr. David Alpan may recommend Phase 1 TMJ Therapy or he may refer you to other therapists.
How do I schedule my first appointment?
There are several ways:
- Call us immediately at one of our offices. The numbers are listed on the top of each page on our website.
- Schedule an appointment online. Just click on “Request an appointment now” at the top of the page, or on the “contact us” tab and you will be directed to the appropriate page.
After scheduling your consultation, click on New Patient Forms to access and complete the new patient documentation. Please bring your completed forms to your first appointment. We look forward to meeting you and helping you every step along the way.
What is the fee for Phase 1 TMJ therapy, TMD therapy or MSD therapy?
During the initial TMJ exam, Dr. Alpan will determine what the best treatment is based on your signs and symptoms and your answers to his questions. If he determines that you will benefit from TMJ therapy he will prescribe 1-3 ninety minute TENS treatments. If your symptoms persist after the 3 TENS treatments Dr. David Alpan will re-evaluate your condition and either recommend Phase 1 TMJ treatment or refer you to other therapists.
How long will I be in MSD, TMD or TMJ therapy?
Nobody can know before treatment starts how long you will need treatment. In some cases, one TENS treatment solves the problem. In others, TENS treatment may last six months. Some patients will require a removable dental splint or mandibular orthodpedic repositioning appliance (MORA) to aid in treatment. When the teeth on the right and left side hit at the same time or when the upper teeth on the right and left side hit the removable dental Splint or MORA at the same time and this relationship holds for a few months without requiring adjustments, TMJ treatment is complete. When signs and symptoms are alleviated or totally eliminated TMJ therapy is finished. In many patients the symptoms are only lessened. TMD treatment is also referred to as “Pain Management.” Some permanent changes caused by TMJ/TMD injury or genetics, etc., may not be reversed with TMJ therapy.
If symptoms can only be lessened, Dr. David Alpan will refer you to other health care providers – a Chiropractor, Osteopath, Cranial Osteopath, Podiatrist, Physical Therapist, Bio-feedback Therapist, Psychologist, Acupressure specialist, Acupuncturist, Massage Therapist, etc. Anyone that works with TMJ/TMD can help you.
Sometimes a team of doctors must treat a patient with TMJ/TMD problems at the same time. The longer the condition has existed, the longer and more expanded the treatment may become. It is for this reason that Dr. David Alpan recommends that every child be examined at age seven (7). Anyone with chronic pain or any of the other TMD-TMJ Signs and Symptoms should be examined as soon as the signs or symptoms are noticed.
After phase I TMJ therapy is completed and most if not all the symptoms have been reduced Dr. David Alpan may recommend Phase II TMJ therapy. Many patients would ask to create a more permanent solution using orthodontics to move the teeth into a position that can support the bite and not create more TMJ/ TMD symptoms. In some patients, surgery may be required.
What happens after MSD, TMD or TMJ therapy?
If all your symptoms are alleviated with 1-3 TENS treatments, then nothing else happens. After Phase 1 TMJ therapy, there are ways to permanently retain the relationship of the lower jaw to upper jaw and skull without the removable dental splint or orthotic.
Some of the alternative ways to accomplish this are:
Orthodontic treatment with tooth braces = Phase 2 TMJ therapy done by Dr. David Alpan or crowns, implants, bridges, partial or full dentures done by your general dentist. Dr. David Alpan does orthodontic treatment in Phase 2 TMJ treatment when you don’t want to continue wearing the removable dental Splint. If you don’t want orthodontic treatment, he will refer you to your general dentist or a specialist if necessary.
After your teeth are moved with orthodontic treatment, the new muscle-skeletal relationship should hold for the rest of your life. You will have to wear a retainer at home and while you sleep for the rest of your life in order to prevent relapse of the moved teeth. Using a retainer after orthodontic treatment is required for everyone. Some clenching and grinding habits may still require a dental night guard long term. We look forward to helping you solve your TMJ/TMD concerns.
Will a retainer be necessary?
No, a retainer is not necessary if we did not move your teeth with orthodontic treatment. If we have completed Phase 2 TMJ therapy, then, yes, a retainer is necessary. Sometimes a dental night guard may be worn long term if a grinding habit still persists with no other TMJ/TMD symptoms or signs.
In most instances, after Phase 1 TMJ therapy is complete, orthodontic treatment (Phase 2 TMJ therapy) can move the teeth in order to maintain the relationship of the lower jaw with the upper jaw and skull so that there is no strain on the muscles of the face that move the jaw when you speak, yawn, chew and swallow. If orthodontic movement of the teeth is used to maintain this relationship, you will have to wear a retainer to prevent relapse of the moved teeth.
Restorative procedures such as dental fillings, dental crowns, dental bridges, partial dentures and full dentures, can also be fabricated to “retain” this muscle skeletal relationship. Sometimes a combination of orthodontic treatment and restorative dental procedures will create the ideal long term “retention.”
Can my family dentist do MSD, TMD or TMJ therapy?
Some general dentists have invested the time and effort to learn about this subject. It is not taught in any of the dental schools. After the dentist graduates from dental school he/she must spend their own time, effort, and money away from their dental practices taking hundreds of hours of postgraduate courses all over the country to gather the data necessary to become a TMJ Therapist.
This is what Dr. Alpan did while in dental school, orthodontic specialty training, and after he graduated as an orthodontist in 1998. During his two years in specialty training to become an orthodontist, he spent hundreds of hours in the TMJ Clinic with Dr. Chase at the UOP School of Dentistry in San Francisco. He took many post-graduate courses on treating TMJ/TMD problems.
Myotronics, founded by Dr. Bernard Jankelson, has been developing sophisticated electronic equipment for TMJ/TMD diagnosis and treatment and instructing courses since the late 1960’s. Dr. Jack Alpan, his father (a general dentist), was trained by Myotronics in 1973. Dr. Jack did TMJ/TMD therapy from 1973-1997 and gave public lectures on this subject that Dr. David Alpan attended during his formative years. Dr. Jack inspired Dr. David regarding the importance of TMJ/TMD diagnosis and treatment for the best practice of general dentistry and orthodontics. That motivated Dr. David Alpan to make the extra effort to learn more about TMJ/TMD diagnosis and treatment.
Dr. David Alpan wrote his Master’s thesis on a TMD research project he did during his two years of orthodontic specialty training. For this he was awarded the Master of Science in Dentistry (MSD) degree. He has been diagnosing and treating patients with TMJ/TMD problems since his graduation as a dentist in 1996 from the UOP School of Dentistry in San Francisco.
Do I still need to see my family dentist?
Yes, you still need to see your family dentist for regular dental check-ups and tooth cleaning. If your family dentist does TMJ/TMD treatment and he referred you to Dr. David Alpan for orthodontic treatment and Dr. David Alpan determines that you need TMJ/TMD therapy, he will refer you back to your family dentist for TMJ therapy.
Even during TMJ therapy your general dentist will monitor your oral health to determine if you need fillings, gum treatments, etc… Dr. David Alpan collaborates with his patients’ general dentists as part of the team effort to provide the best dental health care for each patient.
Do I need to be referred?
No, you do not need to be referred; however, many general dentists do refer their patients to Dr. David Alpan for TMJ/TMD treatment. Dr. David Alpan may also refer you to other specialists if necessary.
What foods do I have to avoid?
During the course of your TMJ/TMD therapy, you may have to wear a clear, plastic, removable dental Splint that fits over your lower teeth. To prevent excessive wear and breakage of this dental Splint, it is best to avoid very hard foods – pop corn, ice crushing, hard nuts, hard candies, etc. When you feel discomfort from eating, don’t eat hard, chewy foods.
If you don’t need a dental Splint, you can eat whatever you want. Of course, sugar and all refined and processed foods are not good for your teeth, gums and jaw bones. Eat whole natural foods (80% raw foods) that have had the least amount of processing as possible. All sweet things promote caries for 98% of the population and bone loss around the teeth for 80% of the adult population.
If you have any more questions regarding TMJ/TMD therapy not covered on this web page, please Contact Us by phone, fax, or email. We will gladly answer your questions. We look forward to seeing you at your Initial TMJ Exam appointment.
Who should get MSD, TMD or TMJ therapy?
What is TMD?
What is TMJ?
What is TMJ Therapy?
What is the fee for the initial TMJ exam, TMD exam or MSD exam?
How do I schedule my first appointment?
What is the fee for Phase 1 TMJ therapy, TMD therapy or MSD therapy?
How long will I be in MSD, TMD or TMJ therapy?
What happens after MSD, TMD or TMJ therapy?
Will a retainer be necessary?
Can my family dentist do MSD, TMD or TMJ therapy?
Do I still need to see my family dentist?
Do I need to be referred?
What foods do I have to avoid?
Ask the Orthodontist (Questions and Answers with Dr. David Alpan)
